At Zenith Medical Billing, our Denial Management Services are designed to streamline your revenue cycle and ensure that your healthcare practice receives the maximum reimbursement for services rendered. We specialize in identifying, analyzing, and resolving claim denials quickly and efficiently, helping to reduce financial losses and improve cash flow.
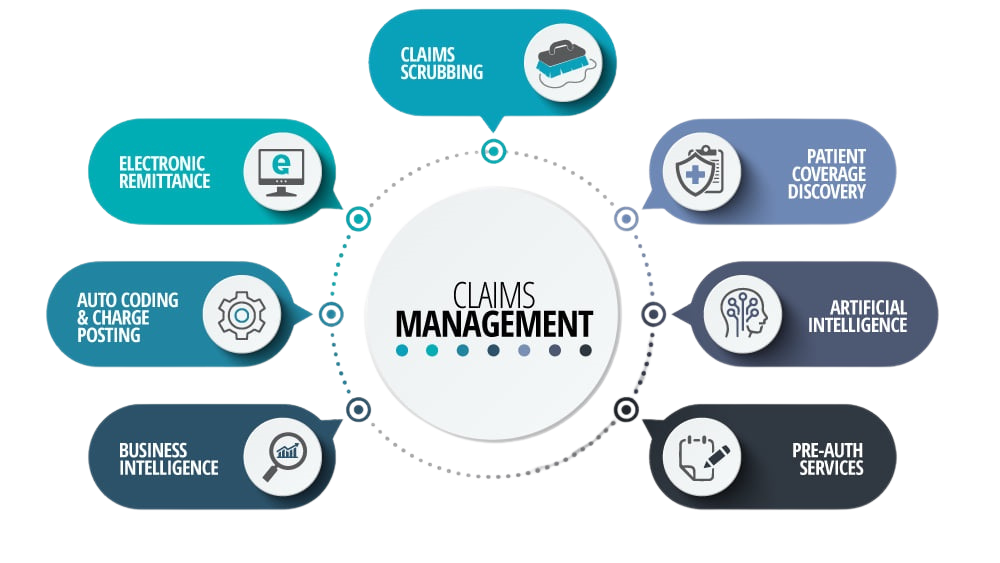
Our expert team works diligently to review all denied claims, uncover the root causes, and implement strategies to prevent future denials. From correcting coding errors and ensuring prior authorizations to verifying insurance eligibility, we take proactive steps to ensure clean claims submissions. With a robust appeals process and advanced reporting tools, we provide clear insights into denial trends and offer solutions that drive better financial outcomes for your practice.
Zenith Medical Billing is committed to helping you reduce your denial rate, improve your first-pass resolution rate, and optimize your revenue cycle, so you can focus on what matters most—providing excellent patient care.